Abstract

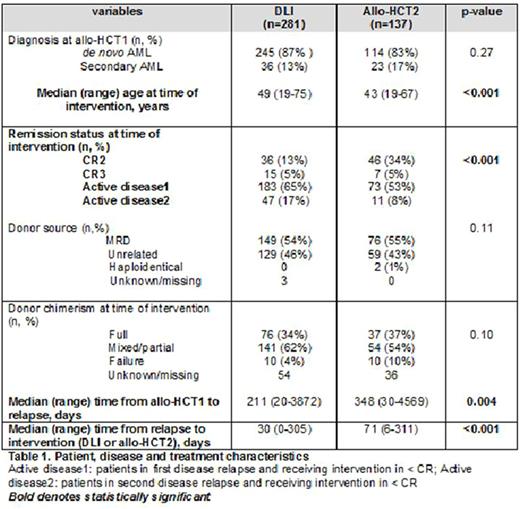
Background: We have previously reported that in patients with acute myeloid leukemia (AML) relapsing after allogeneic hematopoietic cell transplant (allo-HCT) outcome was highly dependent on the use of donor lymphocyte infusion (DLI) or second transplant for consolidation. Despite response to chemotherapy without cellular therapy to consolidate, most of the patients relapsed and died (Schmid C, et al. JCO 2007;25: 4938-4945).There are no randomized controlled trials comparing DLI vs. second allo-HCT (allo-HCT2) for patients with AML relapsing after a first allo-HCT. The decision to offer DLI or an allo-HCT2 is based on several factors including remission status, donor availability, performance status, and center or physician preference. Methods: We conducted a retrospective comparative analysis of 418 patients with post-transplant relapsed AML treated with either DLI (n=281) or an allo-HCT2 (n=137) at 61 EBMT participating centers between 1992 and 2014. Primary endpoint was overall survival (OS). All analyses were performed on an intent-to-treat basis. Results: Patients treated with DLI (n=281) were older (median age 49 vs. 43 years, p<0.001), had shorter median time from first allo-HCT to relapse (211 vs. 348 days, p=0.004), received the intended treatment faster (30 vs. 71 days, p<0.001), but were less likely to be in complete hematologic remission (CHR) at the time of intervention (18% vs. 39%, p<0.001) (Table 1). For patients in the DLI or allo-HCT2 groups the median follow-up for survivors was 64 (1-157) months and 61 (15-110) months, respectively. There were no differences in 5-year OS between treatments [DLI=15% (95% confidence interval (CI):10-19%) vs. allo-HCT2=19% (95%CI:12-25%), p=0.86)]. An analysis of patients who were in complete hematologic remission (CHR) at the time of intervention showed similar 5-year cumulative incidence of relapse [DLI=64% (95%CI:47-77%) vs. allo-HCT2=56% (95%CI:41-68%), p=0.64] and non-relapse mortality (NRM) [DLI=16% (95%CI:7-28%) vs. allo-HCT2=27% (95%CI:16-39%), p=0.08]; and comparable 5-year leukemia-free survival (LFS) [DLI=21% (95%CI:8-33%) vs. allo-HCT2=18% (95%CI:7-28%), p=0.17] and OS [DLI=33% (95%CI:19-48%) vs. allo-HCT2=29% (95%CI:17-42%), p=0.22]. Results in patients with active disease at time of cellular therapy were very poor with 5-year cumulative incidence of relapse being [82% (95%CI:76-86%) vs. 63% (95%CI:52-73%), p=0.02], after DLI or allo-HCT2, respectively. The very high relapse rate resulted in poor 5-year LFS [DLI=10% (95%CI:6-13%) vs. allo-HCT2=6% (95%CI:0-13%), p=0.03], and OS with DLI [DLI=11% (95%CI:7-15%) vs. allo-HCT2=11% (95%CI:4-18%), p=0.59]. NRM was significantly lower with DLI [DLI=9% (95%CI:6-13%) vs. allo-HCT2=31% (95%CI:20-42%), p<0.0001]. Conclusions: There is no difference in 5-year OS when offering DLI versus allo-HCT2 in post-allograft relapsed AML patients. The most important prognostic factor is disease status at time of cellular therapy (whether DLI or allo-HCT2). Best results are achieved in patients who can attain CHR prior to intervention. In patients with active disease results are disappointing with 5-year LFS and OS in only 10% of cases. New therapeutic strategies and novel therapies are needed to improve outcomes in these patients.
Kharfan-Dabaja: Seattle Genetics: Speakers Bureau; Incyte: Speakers Bureau; Alexion Pharmaceuticals: Speakers Bureau. Schmid: Celgene: Research Funding, Speakers Bureau; Novartis: Research Funding, Speakers Bureau; Incyte: Research Funding, Speakers Bureau; MoilMed: Membership on an entity's Board of Directors or advisory committees; Jazz: Membership on an entity's Board of Directors or advisory committees. Mohty: Sanofi: Honoraria, Speakers Bureau.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal